9/28/2023 – Posterior Circulation (PC) Stroke
4.
You are working in TCC. You get a page that reads, “56M w/dizziness, vomiting, ataxia; Spanish-speaking only. Meet at scanner now.”
His vital signs from triage are below:
HR: 70
BP: 150/80 mmHg
RR: 14
O2 sat: 97% RA
T: 37 C
You arrive as the patient is being wheeled to the outside of the CT scanner. He is a middle-aged Hispanic male slumped to one side in the wheelchair who appears very anxious. The patient is intermittently vomiting, cannot sit up straight, and has obvious nystagmus. He does not speak any English.
What would your next steps be?
ABC’s
Check POCT BG
Obtain PIV access
Spanish interpreter to obtain a brief history (focused on symptoms and contraindications to lytic therapy)
Activate stroke pager (for all possible strokes, not probable strokes)
Perform NIHSS
Repeat vitals
Obtain non-contrast CT head, obtain CTA/CTP if NIHSS > 6 OR aphasic
The patient’s BG is 92 mg/dL. A nurse grabs the interpreter iPad, which is unfortunately not charged. While she works on getting the device charged enough to turn on and obtaining interpreter assistance, an EM resident with conversational Spanish skills grabs the brief history and starts to run through TNK contraindications.
Contraindications to TNK include:
Symptom onset greater than 4.5 hours
Intracranial hemorrhage on HCT or history of intracranial hemorrhage
Neurosurgery, head trauma or CVA in last 3 months
Known intracranial AV malformation, neoplasm, aneurysm
Hypertension (>185 / >110 mmHg)
Present use of anticoagulation
- INR must be less than 1.7 to receive lytic
- Anti-factor Xa must be less than 0.15 to receive lytic
- Platelets <100,000
- Active internal bleeding
- Suspected/confirmed endocarditis
You confirm that the symptoms started 2 hours ago (placing him within the <4.5-hour window). CT head is obtained and negative. The NIHSS is 5. Using the interpreter services, you determine he has no contraindications to TNK, so you order and administer weight-based dosing of TNK. The patient is not a candidate for CTA/CTP given his NIHSS and lack of aphasia.
These cases often run very quickly, so some logistics and latent safety threats to consider:
Glucose is a vital sign. We should not be proceeding with a CT until we have ruled out hypo- or hyperglycemia [1].
Interpreters are required by law and essential for good patient care.
Title VI of the Civil Rights Act (specifically, Executive Order 13166) states that those with limited English proficiency are entitled to written and oral translation services [2]
Whenever you walk by them on shift, make sure that interpreter iPads are plugged in and charged. If they are broken, bring them to the Comm center and indicate to the charge RN that they need to be fixed.
If the iPad is broken or not working, call (314) 747-5682. The codes you need are “1000” followed by “800” to access an interpreter in our ED.
Please see attached slides for more info on how to utilize interpreters well!
3. The NIHSS is biased towards patients with anterior circulation strokes. Still call a stroke alert for your patients with suspected posterior circulation (PC) stroke.
Signs and symptoms concerning for PC stroke:
Continuous, non-provoked dizziness/vertigo/lightheadedness, especially combined with acute hearing loss
Spontaneous vertical, purely torsional, or direction-changing nystagmus.
Asymptomatic nystagmus.
Isolated vomiting, dysarthria
Dysmetria, change in speech, and extremity or truncal ataxia [3]
4. Designate a leader and the team. Ideally the ED attending should be delineating clear roles and running the stroke like a trauma or a code.
Too many voices/leaders make things difficult for the CT technician.
Avoid crowding the CT scanner if you are not directly involved in patient care.
5) Closed loop communication is key in these situations where there are many team members working in concert.
Remember to address the individual you are speaking with by name (or any other appropriate identifier, use the color of their scrubs or another descriptor andthen apologize and learn their name after the case).
Confirm the name of the medication, dose with units (milligrams, milliliters, etc.), route (intravenous slow push, infusion, intramuscular, etc.)
Request that the individual receiving the information provides a verbal
confirmation by repeating this information to you.
References:
1. Rodriguez-Hernandez A, Babici D, Campbell M, Carranza-Reneteria O, Hammond T.Hypoglycemic hemineglect a stroke mimic. eNeurologicalSci. 2023 Jan 17;30:100444.doi: 10.1016/j.ensci.2023.100444. PMID: 36698773; PMCID: PMC9869408.
2. Clinicians’ Obligations to Use Qualified Medical Interpreters When Caring for Patients with Limited English Proficiency. AMA Journal of Ethics. 2017;19(3):245-252.
3. Pelletier J, Koyfman A, Long B. Pearls for the Emergency Clinician: Posterior Circulation Stroke. The Journal of Emergency Medicine. Published online July 2023: S0736467923004006. doi: 10.1016/j.jemermed.2023.07.0073 / 3 77%
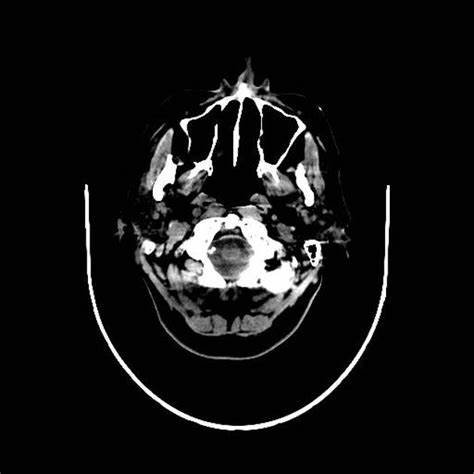
4. Images Posterior circulation stroke | Radiology Case | Radiopaedia.org