10/5/2023 Breech OB
You are working in TCC when you get the following page: “31 y.o female with urge to push to 5R, ETA 3”.
What personnel should be notified? How would you prepare your room?
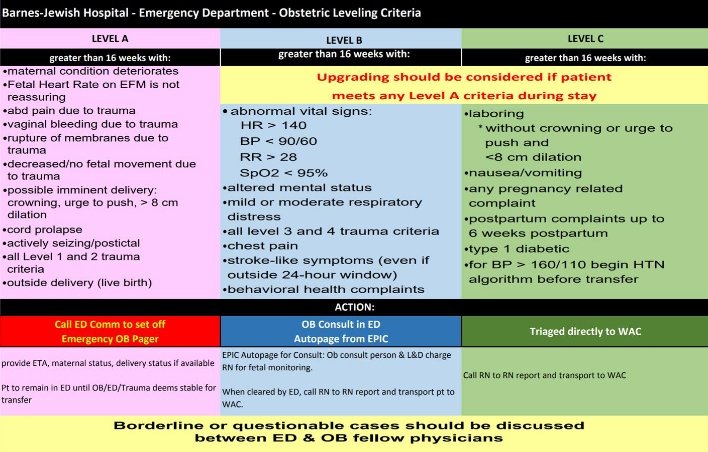
Based on our OB leveling criteria this would be classified as a Level A (urge to push), which means OB and pediatrics will be paged by the comms center and both will come to bedside as soon as possible. However, recall that both services are on the other side of campus in different buildings and thus there is generally about a 10-minute delay before they can get there. If the case is truly emergent or there is new information (breech delivery, cord prolapse or other concerning findings), you may ask the comm center to re-page them to let them know. The OB leveling criteria is below:
In terms of room preparation, the essential items are the obstetrics tray, the infant warmer (Ohio Table), the ultrasound, and the fetal monitoring system. The Infant Warmer (Ohio Table) is kept outside of room 1 in TCC, the back-up warmer is located outside of BHP.
The location of the supplies needed are listed below:
• Precipitous delivery pack – in the cabinet to the left of TCC 5
• C-section pack – on top of cabinet to the left of TCC 5
• C-section instrument tray – in the cabinet to the left of TCC 5
• Tocometry is under the TCC Desk
The patient arrives in TCC. She is screaming in pain and having active contractions. Her vital signs are below:
BP: 120/70
HR: 110
RR: 20
O2 sat: 97% RA
T: 36.8 C
You attempt to obtain a history from her. She is a G5P4 She reports that she does not know her gestational age but says that her LMP was about 9 months ago. She has been unable to receive prenatal care. She has no medical history. She felt her water break about 30 minutes ago and is having contractions every few minutes. She continues to yell out in pain.
What is your next move?
You can now proceed to assess for crowning. If you don’t already feel the baby’s head, it would be helpful to perform a bedside ultrasound to see the presentation of the fetus. If the baby is breech, then re-page OB to let them know.
It is important to note that it can take between 8-12 minutes for teams to arrive from Parkview Tower, once paged. If baby is already crowning, you may be performing the delivery without OB present.
You examine the patient and perform a bedside ultrasound. You are able to palpate the fetal presenting part but are unsure if it is the head or buttocks. On your ultrasound you confirm that baby is in breech position. You ask nursing to apply the fetal heart monitor and see that baby’s heart rate is 140.
It is important to figure out which type of breech presentation the baby is in. Frank breech is a baby with flexed hips and legs directed towards the face in a pike position. In frank breech the thigh, trunk/buttocks are the presenting parts. In complete breech the baby is in a sitting position with both hips and legs flexed. This has the buttocks/trunk, thighs and legs presenting. Incomplete breech on the other hand is where the fetal feet/leg(s) are the presenting part. In incomplete breech, the presenting feet generally pass easily through an incompletely dilated cervix. However, the head may not pass as easily, and thus incomplete breech carries a high risk of head entrapment and subsequent complications. Importantly, frank breech or complete breech can be delivered vaginally, however incomplete breech is a contraindication to vaginal delivery for singleton pregnancies. If you feel a fetal foot as the initial presenting part, notify OB immediately as the patient likely needs to go for a Cesarean section.
You conclude that baby is likely in either frank or complete breech as you palpate buttock. OB is on their way and you repage them to let them know. You move the patient towards the end of the bed to optimize positioning.
How would you control her pain?
Pain control in a patient about to deliver is challenging. Administration of IV opioids may be effective for controlling mother’s pain, however they cross the placenta and can increase the risk of neonatal respiratory depression. If opioids are given, shorter acting agents (fentanyl, remifentanil) are preferred. Non-steroidal anti-inflammatory drugs should be avoided as they can precipitate premature closure of the ductus arteriosus. Acetaminophen is an option but may not have sufficient potency. The use of nitrous oxide is common in other countries but not widely used in the US. Ketamine has been proposed as an option however there is not robust data on its safety or effectiveness for this use.
What is your next step? How would you deliver baby while awaiting obstetrics?
Although it may be tempting to “help” with the initial portion of the delivery, during the first part of a breech delivery it is important not to apply pressure or traction on the presenting part as this contributes to cervical dilation and is necessary to increase the probability that the fetal head will successfully pass.
Once the umbilicus is visible then it safe to begin assisting with suprapubic pressure and if needed, gentle rotational force can be applied to help deliver the legs. Once the cord is exposed, a small loop can be created to avoid cord traction during the delivery. Generally, the shoulders and arms will deliver spontaneously; however if there was traction applied initially, this can lead to challenges at this point in the delivery. If traction is needed at this point in the delivery, care should be taken to grip the pelvis or bony structures and avoid pressure on the abdomen or other solid organs to avoid injury. Rotation and gentle traction can be helpful to deliver the arms, however it is possible you will need to sweep the arms through using a finger in the antecubital fossa.
As opposed to cephalic vaginal births, the head is delivered with flexion in the breech delivery. For delivering the head, one hand can be placed on the rostral side with the fingertips over the maxilla, while the other is placed on posterior thorax to stabilize the neck. Care should be taken to keep the neck in a neutral position and avoid excessive flexion or extension. Head entrapment is more common in preterm birth and often requires specialist intervention. While awaiting obstetrics assistance, the McRoberts position combined with a uterine relaxant such as Terbutaline can be administered.
Obstetrics and pediatrics arrive while the buttocks is emerging. You give a focused handoff describing mother’s G/P status, important comorbidities, dates, and labor progress. Prior to delivery and the patient has an uneventful breech delivery. The placenta is delivered shortly afterward. Pediatrics attends to baby who is stable as well. Mother and baby are transported to labor and delivery without issue.
References:
1) American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 209: Obstetric Analgesia and Anesthesia. Obstet Gynecol. 2019;133(3):e208-e225. doi:10.1097/AOG.0000000000003132.
2) Mattingly JE, D'Alessio J, Ramanathan J. Effects of obstetric analgesics and anesthetics on the neonate: a review. Paediatr Drugs. 2003;5(9):615-627. doi:10.2165/00148581-200305090-00004
3) Joel S, Joselyn A, Cherian VT, Nandhakumar A, Raju N, Kaliaperumal I. Low-dose ketamine infusion for labor analgesia: A double-blind, randomized, placebo controlled clinical trial. Saudi J Anaesth. 2014;8(1):6-10. doi:10.4103/1658-354X.125897
4) Hofmeyr J. Delivery of the singleton fetus in breech presentation. UpToDate. https://www-uptodate-com.beckerproxy.wustl.edu/contents/delivery-of-the-singleton- fetus-in-breech-presentation search=breech&topicRef=6776&source=see_link#H7. Published July 13, 2023. Accessed October 14, 2023.
5) Hofmeyr J. Overview of Breech Presentation. UpToDate. https://www-uptodate- com.beckerproxy.wustl.edu/contents/overview-of-breech- presentation?search=breech&source=search_result&selectedTitle=1~92&usage_type=de ault&display_rank=1. Published July 14, 2023. Accessed October 14, 2023.